Blogs
In 2021, the World Health Organization (WHO) estimated 247 million malaria cases and 619,000 malaria deaths globally. Most of this burden befell Africa, where children less than 5 years of age and pregnant women were the most affected.
Malaria prevention strategies face many threats, including resistance of malaria parasites to antimalarial drugs, vector resistance to insecticides, and missed malaria infections due to the inability of often trusted rapid diagnostic tests (RDTs) to detect the Plasmodium falciparum parasite. An additional threat is the funding gap for malaria, where the money invested in malaria control and elimination efforts is far less than the resources needed. Furthermore, service disruptions from pandemics such as COVID-19 and other humanitarian/health emergencies are major drawbacks in the malaria elimination efforts. Importantly, an invasive mosquito species, namely Anopheles stephensi, entered Africa in the last decade. This invasive species, which is considered an efficient urban malaria vector, is reported to be resistant to many of the insecticides used in public health, thereby posing an added challenge to malaria elimination efforts on the continent.
mAbs recommendation for malaria prevention
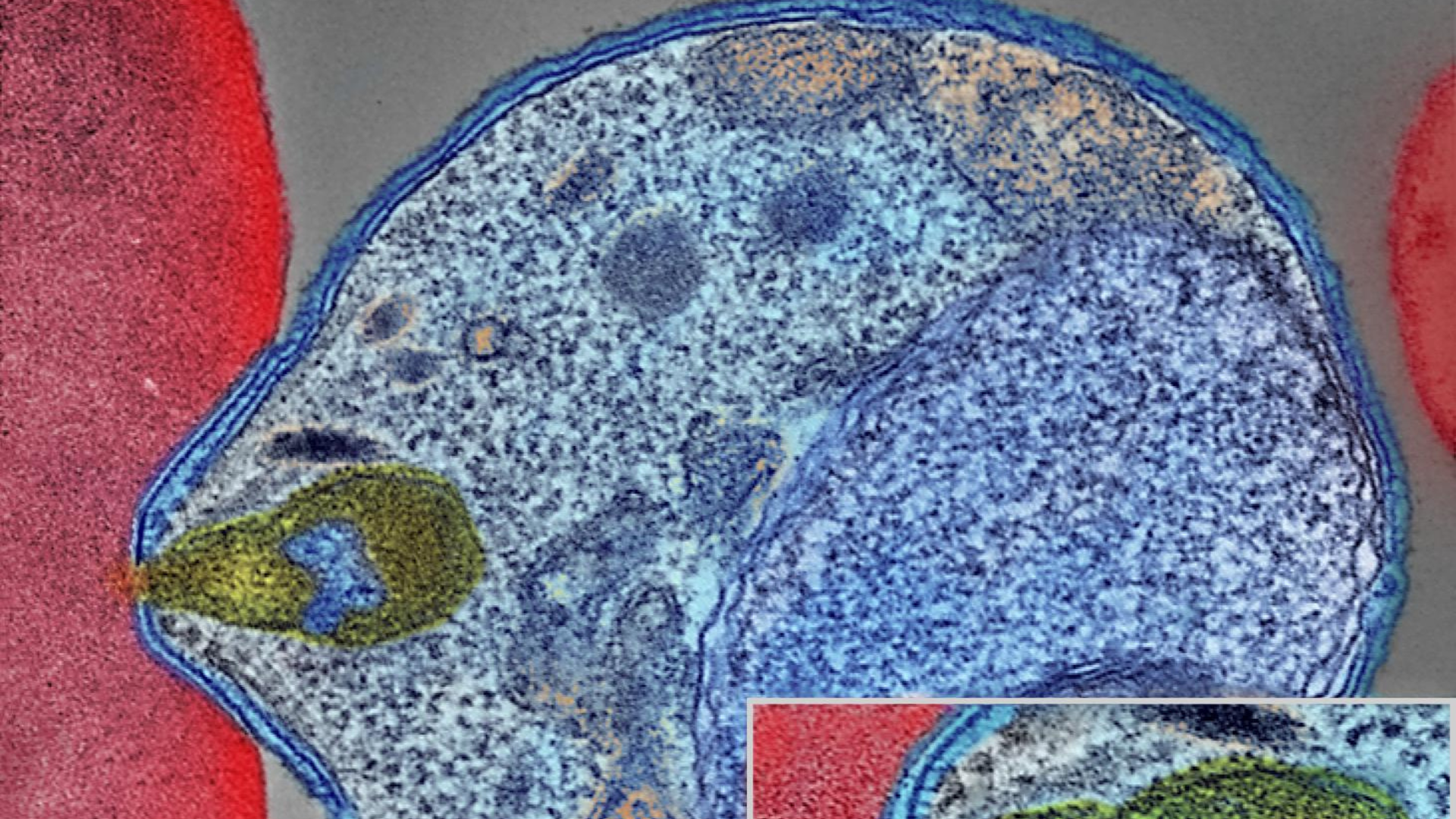
The WHO Global Malaria Programme has recommended the need to intensify research and development of new technological tools with the ability to take us to elimination. Among these new tools being developed are monoclonal antibodies (mAbs). Monoclonal antibodies work through preventing the multiplication of the parasites in the blood and decreasing the number of parasites hence averting clinical disease.
Early-stage clinical trials for malaria mAbs conducted in Mali and Kenya have shown promising results, including demonstrated high efficacy, safety and tolerability. For example, the clinical trial conducted in Mali in 2021 found the mAbs to be protective against P. falciparum infection with 88.2% efficacy over a 6-month malaria season without evident safety concerns.
Potential gains for mAbs use in malaria prevention
There are several reasons why the addition of mAbs to the malaria control arsenal will be a good thing. First, mAbs could be used to provide protection from malaria in cases where there is increased antimalarial drug resistance. Secondly, being a single-dose application coupled with the fact that they will potentially confer protection over a longer period of time (up to 6 months or more) gives mAbs an edge over currently used antimalarial drugs, which have a complex drug regimen with potential adherence issues. Thirdly, mAbs offer higher efficacy (88.2%) in comparison to the current WHO-recommended RTS, S/AS01 vaccine, which has moderate efficacy of approximately 30%. Additionally, mAbs compare better to the next generation R21/Matrix-M vaccine, which recorded a 74% efficacy rate from a randomised control trial. What is more, is that mAbs have a single-dose regimen compared to the three-dose regimen for the R21 malaria vaccine.
Barriers to mAbs use and access in Africa
Globally, there is only a handful of licenced mAbs for infectious diseases such as scabies, Ebola and respiratory syncytial virus (RSV). However, there is very limited access to mAbs in Africa, with the continent having only 20% of the mAbs market compared to 80% in high-income countries in other continents. The challenges hindering access to mAbs in Africa include: (a) lack of awareness by governments and policymakers on the broad potential that mAbs offer to treat and prevent diseases, (b) lack of capacity by drug and pharmaceuticals regulators in evaluating the mAbs for market authorization, (c) variation in the drug and pharmaceuticals registration requirements with very long wait times across national authorities, making the African market unattractive for manufacturers, and (d) high prohibitive costs occasioned by expensive manufacturing processes limit mAbs availability to the small segment of the population can afford them.
Increasing mAbs access in Africa
There is an urgent need to increase awareness of the potential of mAbs in preventing and treating malaria. Engaging in advocacy efforts will potentially lead to deliberate conversations and actions on prioritisations, commitments and investments in mAbs by African governments and policymakers.
To address the regulatory capacity constraints, collaborative partnerships with accomplished regional institutions such as the African Vaccine Regulatory Forum (AVAREF) will serve to strengthen and sustain the regulatory capacity of biological products through training and harmonization of drug and biopharmaceutical product assessments prior to market authorization.
Strategies to lower the high cost of mAbs include the inclusion of mAbs into the WHO Essential Medicines List (EML), which is a prerequisite step for theWHO prequalification that is used by many countries to guide bulk purchases. This then makes the products available through the national public health systems. Additionally, utilizing business models such as public-private partnerships may bolster local manufacturing and increase investments needed to stimulate industry focus on delivering affordable and accessible mAb products in Africa.

